Abstract
Objective
To study endothelial injury from a newly designed asymmetric double port Descemet Membrane Endothelial Keratoplasty (DMEK) injector, both ex-vivo and in clinical practice.
Design
Laboratory investigation with an interventional case series study.
Method
Sixteen rabbit endothelial rolls were tested for injection using a no-touch technique. For each pair of rolls, one endothelial graft underwent injection with a single port Pasteur pipette twice, wheras the other was injected with a novel asymmetric double port injector with a larger diameter entry port than the exit port also twice. Each graft was stained with 4-6-diamidino-2-phenylinidole dihydrochloride and was counted under a fluorescence-inverted microscope before and after injection. The proportion of graft injury was calculated and the differences were analyzed. Subsequently, six patients requiring DMEK underwent surgery using this novel insertion device and endothelial cell loss was calculated 3 months after the surgery.
Results
After injection, the mean proportion of endothelial cell survival with the single port pipette was 78.8% (n=8; SD: ±20.9%), whereas the double port injector yielded a survival rate of 96.8% (n=8; SD: ±8.4%). This difference was statistically significant (P=0.008), representing less endothelial injury with the double port device. Early endothelial cell loss after 3 months in the DMEK patients was 26.1% (SD: ±6.1%).
Conclusion
In our injection model, using a double port injector created significantly less endothelial cell damage than with the single port pipette. Clinically, this device yielded early endothelial cell loss comparable to that of the series performed by experienced DMEK surgeons.
Similar content being viewed by others
Introduction
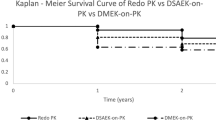
Descemet Membrane Endothelial Keratoplasty (DMEK) has enjoyed a rapid increase in popularity in recent years.1 Although endothelial cell loss may be higher during the learning curve,2 larger series of cases3, 4 have reported similar results as DSAEK (Descemet Stripping Automated Endothelial Keratoplasty).
Tissue delivery into the eye is responsible for some of the endothelial cell loss observed postoperatively. Minimizing tissue touch, friction, and compression is essential for reducing trauma.5
In the current article, we describe a newly designed asymmetric double port DMEK injector and evaluate our preclinical and clinical data.
Methods
Injector design
The injector is made of glass and it is not reusable. It consists of a glass pipette that has a proximal end with a 3 mm diameter lumen in, where all the tubing and syringe that allows suction and ejection of air/fluid are connected; and a 0.8 mm diameter lumen distal end, which is the tip where the graft exits the injector into the eye (Figure 1). This pipette is a hollow cylinder but as it approaches the tip, it suddenly becomes a conical-shaped trunk, progressively diminishing its diameter from 3 mm to 0.8 mm. This allows progressive rolling of the graft as it advances through the pipette to permit its exit through the small diameter port. The tip of this port can be inserted into a standard cataract surgery incision of 2.8 mm.
Artistic impressions of the insertion of the DMEK graft. (a and b), the graft is loaded by a suction force through the large port while occluding the small port. (c and d), the graft is pushed along the small port, the double roll should be facing up inside, (e and f) the injector is positioned into the main incision to insert the DMEK roll into the recipient anterior chamber. After insertion, the double roll should still be facing up.
Approximately in the distal one-third of the pipette, an accessory conical-shaped glass trunk/port is connected to the main trunk, connecting its lumens. This accessory conical-shaped port has a lumen diameter of 4 mm and forms an angle of 70° with respect to the main trunk/pipette (Figure 1). The mechanism of suction and injection of the graft is explained below in the DMEK surgery section.
Ex-vivo laboratory study
Sixteen eyes of New Zealand (NZ) white rabbits were used. The procedures were approved by the Animal Welfare Committee of La Paz University Hospital, Madrid. The endothelial rolls from the NZ white rabbits’ corneoscleral rim were obtained by direct peel under immersion, using a modified SCUBA (submerged corneas using backgrounds away) technique.6 The detached DM scrolls with the endothelium on the outside.
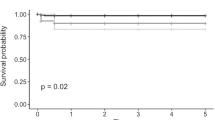
Endothelial rolls were stained with 4-6-diamidino-2-phenylinidole dihydrochloride (Sigma, St Louis, MO, USA) for 5 min, and the nuclei were counted under a fluorescence-inverted microscope (Nikon, Tokyo, Japan). Drops of saline were poured into the endothelial roll placed on a glass slide to allow complete or partial central unrolling. A central area of 0.5 mm2 was examined with a × 40 objective and the non-apoptotic nuclei were counted before and after passing twice through the double port injector or a Pasteur pipette for comparison. Eight rabbit endothelia were used randomly and blind for each type of injector. Student’s t-test was used to assess statistical significance at P<0.05 (Figure 2).
Interventional case report
Following analysis of the ex-vivo data, the first six consecutive cases (one man and five women) who underwent DMEK at the Cornea Unit of University Hospital Ramón y Cajal, Madrid using the final design of our injector, were included in a prospective study for the analysis of endothelial cell loss. The study was approved by Institutional Review Board, and informed consent was obtained from each participant. The average age of the patients was 65 years (SD: 12). Indication for surgery was endothelial decompensation due to Fuchs endothelial dystrophy, with one case of pseudophakic bullous keratopathy. All eyes were pseudophakic. One patient underwent bilateral DMEK. FAM performed all surgical steps and had long experience in DSAEK surgery and had done 12 previous DMEK.
Donor tissue preparation
The SCUBA technique was used. Trephination was 8.25 (n=2) or 8.0 (n=4).
DMEK surgery
All eyes underwent prophylactic inferior iridectomy 1 month before the DMEK surgery. Retrobulbar anesthesia was used in all the patients.
A self-sealing 3.0 mm clear corneal incision at the temporal side and two-side-port at the superotemporal and inferotemporal quadrant are made. A descemetorhexis is performed under air and the host DM is removed. The roll, which had been placed on a watch glass stained with 0.06% trypan blue dye and submerged in HBSS, is gently introduced through the port with the larger lumen by aspiration with the syringe, connected to the glass injector with plastic tubing, while occluding the port with the smaller lumen (Figure 1 and Supplementary Video 1). Once the roll is aspirated up to the intersection of both ports, the larger lumen is occluded and the roll is pushed down the pipette using the syringe to the tip of the port with the smaller lumen (Supplementary Video 1). The injector is inserted into the anterior chamber and the roll is delivered by pressing the plunge of the syringe. The main incision is secured with a single 10/0 nylon suture. After confirming the correct orientation of the graft using the Moutsouris sign1 with a spatula, a small air bubble is injected beneath the donor and it is unfolded and centered using gentle strokes on the corneal surface. The air bubble is then expanded to fill the anterior chamber, and intraocular pressures of around 30 mm Hg are obtained. The patient is instructed to remain supine for 24 h. Two hours after the surgery, the patient is checked for pupillary block.
Data collection
The preoperative endothelial cell density (ECD) of the donor was provided by the Eye Bank using the Konan cell analyzer (Konan Medical Inc., Tokyo, Japan). The postoperative ECD analysis was performed 3 months after surgery. The endothelium was evaluated using a Topcon SP3000p noncontact autofocus specular microscope (Topcon Co., Tokyo, Japan). Images of the central corneal window were analyzed and manually corrected and three measurements of ECD were averaged.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers/animals were followed during this research.
Results
Ex-vivo
The double port injector supported a statistically better cell survival than the one-way injector (Figures 2, P=0.008), with endothelial cell survival of 96.8% (SD: 8.4) vs 78.8% (SD: 20.9), respectively.
Interventional case reports
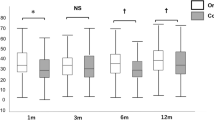
The mean endothelial cell count before dissection was 2526 cells/mm2 (SD: 58.6). Three months after surgery, the mean endothelial cell count was 1892 cells/mm2 (SD: 180.2). The mean reduction at 3 months was 26.1% (SD: 6.1%).
Discussion
The goals of any type of endothelial keratoplasty technique are to improve visual acuity and quality and to provide an ECD high enough to assure long-term graft survival.
Despite concerns that DMEK donors are subjected to greater manipulation and therefore greater endothelial trauma, large series from experienced surgeons have shown endothelial cell loss in DMEK ranging from 34–40% at 6 months, which is comparable to other series of endothelial cell loss in DSAEK.4, 7 Furthermore, fellow eye comparison studies between DSAEK and DMEK did not show differences.8, 9
Endothelial trauma during surgery can be inflicted during donor graft preparation, insertion, and intraocular unwrapping and positioning.
Graft insertion is an important step in determining endothelial survival. Yet, there are no studies comparing devices. Many authors use devices that were not meant for DMEK, particularly plastic IOL cartridges.3, 10 This technique requires grabbing the roll with a forceps to place it into the cartridge. Entrapment of the roll between the wall of the cartridge and the plunger or adhesion of the endothelium to the plastic can produce additional endothelial trauma. Moreover, viscoelastic agents are usually necessary and can interfere with endothelial attachment.11 Dapena et al1, 4 described a no-touch technique for DMEK that uses either a conventional Pasteur glass pipette or a custom-made glass injector. No viscoelastic agent is needed and the glass surfaces are much smoother and can be manufactured without sharp molding edges.1 A drawback of the Pasteur glass pipette is that the small exit port is also the entry port, so the roll needs to be compressed to enter the pipette, with evident friction trauma. The custom-made glass injector of Melles does have a large entry in one end to reduce friction and a small exit in the other end to reduce the size of the incision, but it needs to be disassembled from the syringe when changing from aspirating to injecting the roll, complicating the maneuver. We have designed an injector with a separate asymmetric double port with a large diameter lumen (3–4 mm) and a small diameter lumen (0.8–1.3 mm), not needing disassembling. In our ex-vivo study, we found that a single port pipette produces a significantly higher endothelial cell loss with respect to the double port designed injector. Extrapolating these results, we found that in the first six consecutive cases using the latest version of this device, the early endothelial cell loss attributed to surgical trauma was at least as good as other published series from experienced DMEK surgeons.3, 4, 9
As with other ophthalmic surgeries, the DMEK technique continues to evolve, and the customization and refinement of the injector devices may minimize the endothelial injury from the mere act of insertion. The glass injector allows for minimal manipulation of the tissue and the asymmetrical double port devices may reduce friction during aspiration of the roll compared with single port injectors.

References
Dapena I, Moutsouris K, Droutsas K, Ham L, van Dijk K, Melles GR . Standardized ‘no-touch’ technique for descemet membrane endothelial keratoplasty. Arch Ophthalmol 2011; 129 (1): 88–94.
Droutsas K, Giallouros E, Melles GR, Chatzistefanou K, Sekundo W . Descemet membrane endothelial keratoplasty: learning curve of a single surgeon. Cornea 2013; 32 (8): 1075–1079.
Price MO, Price FW Jr. . Descemet’s membrane endothelial keratoplasty surgery: update on the evidence and hurdles to acceptance. Curr Opin Ophthalmol 2013; 24 (4): 329–335.
Ham L, van Luijk C, Dapena I, Wong TH, Birbal R, van der Wees J et al. Endothelial cell density after descemet membrane endothelial keratoplasty: 1- to 2-year follow-up. Am J Ophthalmol 2009; 148 (4): 521–527.
Bahar I, Kaiserman I, Sansanayudh W, Levinger E, Rootman DS . Busin guide vs forceps for the insertion of the donor lenticule in descemet stripping automated endothelial keratoplasty. Am J Ophthalmol 2009; 147 (2): 220–226 e1.
Giebel AW, Price FW . Descemetis membrane endothelial keratoplasty: the bare minimum. In: Price FW, Price MO editors. DSEK: What You Need to Know About Endothelial Keratoplasty. Slack Incorporated: Thorofare, NJ, 2009 pp 119–146.
Price MO, Price FW Jr . Endothelial cell loss after descemet stripping with endothelial keratoplasty influencing factors and 2-year trend. Ophthalmology 2008; 115 (5): 857–865.
Guerra FP, Anshu A, Price MO, Price FW . Endothelial keratoplasty: fellow eyes comparison of Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty. Cornea 2011; 30 (12): 1382–1386.
Tourtas T, Laaser K, Bachmann BO, Cursiefen C, Kruse FE . Descemet membrane endothelial keratoplasty versus descemet stripping automated endothelial keratoplasty. Am J Ophthalmol 2012; 153 (6): 1082–1090 e2.
Kruse FE, Laaser K, Cursiefen C, Heindl LM, Schlotzer-Schrehardt U, Riss S et al. A stepwise approach to donor preparation and insertion increases safety and outcome of Descemet membrane endothelial keratoplasty. Cornea 2011; 30 (5): 580–587.
Nieuwendaal CP, Lapid-Gortzak R, van der Meulen IJ, Melles GJ . Posterior lamellar keratoplasty using descemetorhexis and organ-cultured donor corneal tissue (Melles technique). Cornea 2006; 25 (8): 933–936.
Acknowledgements
This work was supported in part by grants EC11-139 from the Ministry of Health and Social Politics, Spain; SAF2010-19230 from the Ministry of Economy and Competitiveness, Spain; and from the BioMedical Foundations Mutua Madrileña and Marató TV3, Spain. We wish to acknowledge Juliette Siegfried (ServingMed.com) for the English editing of this manuscript. This work was also supported by grants to F.A.-M. from DGTATX, Ministerio de Sanidad y Consumo (Proyecto TRA-036 y EC11-139), and Fundación Mutua Madrileña, Spain. The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Arnalich-Montiel F and De Miguel M.P hold the patent of the device. The remaining author declares no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Arnalich-Montiel, F., Muñoz-Negrete, F. & De Miguel, M. Double port injector device to reduce endothelial damage in DMEK. Eye 28, 748–751 (2014). https://doi.org/10.1038/eye.2014.67
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.67