But findings apply only to middle-aged or older men with confirmed hypogonadism
Testosterone replacement therapy was not associated with an increase in major adverse cardiovascular events compared with placebo in the large TRAVERSE study of middle-aged and older men with documented hypogonadism and preexisting or a high risk of cardiovascular disease. So reported Cleveland Clinic investigators at the Endocrine Society’s ENDO 2023 meeting in Chicago on June 16. Results of the multicenter study were simultaneously published online in the New England Journal of Medicine.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These findings provide reassurance about the cardiovascular safety of testosterone therapy over the typical duration of treatment in men in whom it is indicated,” says co-principal investigator A. Michael Lincoff, MD, Vice Chair for Research in Cleveland Clinic’s Department of Cardiovascular Medicine. He notes that those are middle-aged or older men with symptoms of hypogonadism and at least two separate properly measured serum testosterone concentrations < 300 ng/dL.
He and his co-investigators emphasize that the cardiovascular safety findings are limited to that population, not to men who do not have indications for testosterone therapy but who nevertheless may receive it through “low T centers” or other unscrupulous prescribers. “This study should not be used as a justification for the widespread prescription of testosterone to aging men,” says study chair Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular & Thoracic Institute.
The TRAVERSE study was prompted by a 2015 FDA requirement that manufacturers of FDA-approved testosterone therapies conduct clinical trials to evaluate whether their products are associated with an elevated risk of cardiovascular events.
“There had been years of conflicting evidence from small trials and observational studies about whether or not testosterone replacement conferred increased risk of myocardial infarction, stroke and other adverse cardiovascular events,” explains Dr. Lincoff, who served on the FDA advisory committee that recommended the requirement. “No well-designed prospective studies of sufficient size and duration had been completed to address this question.”
In response to the FDA mandate, a consortium of testosterone product manufacturers provided funding for the phase 4 TRAVERSE study, which was overseen by the Cleveland Clinic Coordinating Center for Clinical Research (C5Research).
The study was designed as a noninferiority, event-driven safety trial that randomized more than 5,200 men aged 45 to 80 years in a double-blind manner to daily transdermal 1.62% testosterone gel or matching placebo gel. All enrollees had preexisting cardiovascular disease or a high risk of cardiovascular disease and reported at least one of the following symptoms of hypogonadism:
All participants also had to have two fasting serum testosterone results below 300 ng/dL from morning blood draws separated by at least 48 hours. “These are men with documented mild to moderate hypogonadism,” Dr. Lincoff notes. Those with congenital or severe hypogonadism (testosterone < 100 ng/dL) were excluded.
Current cardiovascular disease was considered clinical or angiographic evidence of coronary artery disease, cerebrovascular disease or peripheral artery disease. High cardiovascular risk was defined as having three or more of the following risk factors: hypertension, dyslipidemia, diabetes, current smoking, stage 3 chronic kidney disease, elevated high-sensitivity C-reactive protein, age > 65 years or an Agatston coronary calcium score above the 75th percentile for the patient’s age and race.
Randomization was 1:1 and stratified to ensure equal representation of preexisting cardiovascular disease and cardiovascular risk factors between the two treatment groups. Participants had frequent monitoring of testosterone levels throughout the study period (at 2, 4, 12 and 26 weeks and at 12, 18, 24, 36 and 48 months). Testosterone dose was titrated to maintain testosterone levels of 350 to 750 ng/dL and hematocrit less than or equal to 54%. Sham titrations were done in the placebo arm to maintain blinding.
The primary endpoint was a composite of cardiovascular mortality, nonfatal myocardial infarction or nonfatal stroke. The secondary endpoint was a composite of the primary endpoint plus coronary revascularization. Demonstration of noninferiority was determined to require an upper limit of less than 1.5 for the 95% confidence interval (CI) of the hazard ratio among patients receiving at least one dose of drug or placebo.
Among the 5,204 randomized patients, the mean length of treatment was 21.7 ± 14.1 (SD) months and mean follow-up was 33.0 ± 12.1 months.
The primary endpoint occurred in 182 patients (7.0%) in the testosterone group and 190 patients (7.3%) in the placebo group (hazard ratio = 0.96; 95% CI, 0.78-1.17; P < 0.001 for noninferiority). Rates of the secondary endpoint and each of the components of the primary endpoint were similar between the groups. Findings remained similar in sensitivity analyses that censored events at various time points after drug or placebo discontinuation.
Among adverse events reported, three occurred at a significantly higher incidence with testosterone relative to placebo: atrial fibrillation (3.5% with testosterone vs. 2.4% with placebo), acute kidney injury (2.3% vs. 1.5%, respectively) and pulmonary embolism (0.9% vs. 0.5%, respectively).
“This study shows that, for men with adrenogen deficiency in whom testosterone is clinically indicated, testosterone appears to be safe from a cardiovascular perspective, but it is not without adverse effects,” says Dr. Nissen. He notes that the elevated rates of atrial fibrillation and acute kidney injury had not been reported in previous studies of testosterone, although the increase in pulmonary embolism is consistent with prior studies.
“Our findings support current guidelines that testosterone should be used with caution in men who have had previous thromboembolic events,” the authors write in their study report.
Notably, 61.4% of patients in the testosterone group and 61.7% of those in the placebo group discontinued treatment before the end of the study period. Overall, 20.8% of patients withdrew from the study before end-of-trial visits began. The authors acknowledge these adherence and retention rates as a study limitation, but they note that both discontinuation and withdrawal rates were highly similar between the groups and outcomes data were available for 82.7% of the possible follow-up period.
“While these rates are lower than in most cardiovascular outcome trials,” Dr. Lincoff says, “they are similar to rates in other studies of testosterone and treatments for other chronic symptomatic conditions, such as menopausal symptoms or chronic pain, where patients may choose to change treatments in an effort to gain greater symptom relief. The study’s mean treatment duration of 22 months is common for this condition and is clinically relevant.” He adds that the consistency of the primary findings across various on-treatment sensitivity analyses also reinforces the noninferiority conclusions.
Dr. Lincoff also cites the study’s size as a strength, noting that the 372 adjudicated primary endpoint events observed in this trial exceeded the number in all prior randomized trials of testosterone combined. “This is the most definitive answer to this research question we are likely to get,” he says.
That makes it essential that the findings be interpreted appropriately and not applied to patient populations beyond middle-aged and older men with documented hypogonadism and established cardiovascular disease or high cardiovascular risk. “They don’t apply to athletes taking super-high doses or to people who don’t have low testosterone levels,” Dr. Lincoff says.
Dr. Nissen also stresses that these results came from a setting where patients had their testosterone levels carefully monitored, with drug doses adjusted accordingly. “It’s unclear how often this degree of monitoring happens in general practice, to avoid excessive dosing,” he says. “It’s not likely to be happening in low T centers, where some men don’t even get a baseline testosterone measurement. Testosterone has adverse effects. What if someone with a history of atrial fibrillation or kidney dysfunction or thromboembolism gets it? This therapy is not without risks, especially when not used as indicated. It’s imperative that physicians and the public understand that.”
The study was supported by AbbVie, Acerus Pharmaceuticals, Endo Pharmaceuticals and Upsher-Smith Laboratories.
Radiofrequency ablation significantly reduces symptom severity, shrinks nodules

Maternal-fetal medicine specialists, endocrinologists and educators team up

Giving young patients a hand as they take charge of their own health

Case illustrates how easily condition can mimic preeclampsia
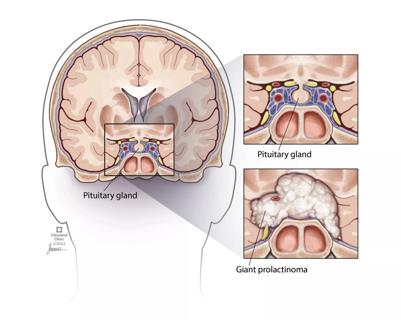
Analysis examines surgical resection of rare pituitary tumors
Screening and medication key to better outcomes

Spinal cord stimulation can help those who are optimized for success
Incidence, outcomes and management